Περιεχόμενα Άρθρου
The global probiotic market is now worth billions of dollars.Credit: d3sign/Getty Images
When she had her daughter in 2008, microbiologist Deanna Gibson rarely saw probiotics in the baby formula on supermarket shelves. “Then when I had my son in 2012, it was pretty much in every formula,” recalls Gibson, who is at the University of British Columbia in Kelowna, Canada. “And there certainly wasn’t the science for it.”

Nature Outlook: The human microbiome
Probiotics — live microorganisms, typically bacteria and yeasts, that are intended to improve health — have intrigued scientists for more than a century, but interest has grown dramatically over the past decade. Their potential for treating or preventing a range of diseases, coupled with their apparent safety, has made probiotics an enticing and lucrative industry that is only expected to grow.
But in 2023 — a year in which the global probiotic market was worth an estimated US$87.7 billion — a preterm baby who was given a probiotic in hospital developed sepsis caused by the same bacteria that was in the product. The baby died shortly after. In response, the US Food and Drug Administration (FDA) issued warning letters to two companies — one of which sold the product given to the baby — for illegally selling probiotics to treat or prevent disease in preterm infants. Although the death is an extreme example of the potential harm that can be caused by probiotic supplements, it has focused some minds. “Bacteria are powerful. That’s why I worry so much about infants,” says Gibson, “and us influencing the microbiome in ways that could have unintended consequences.”
Probiotics are just one category of intervention being used to assess and adjust the community of microorganisms that inhabit a child’s gut. Transplants of faecal matter — an established therapy for adults — are gaining traction for children, despite regulatory impediments. And a growing number of direct-to-consumer microbiome tests are placing data and advice directly in the hands of parents. As scientists and physicians move the field forward, many are focused on not just the potential benefits to children, but also the risks that underlie these interventions. “We’re in the infancy of this field,” says Stacy Kahn, a gastroenterologist at Boston Children’s Hospital in Massachusetts. “We’re not refined enough. We’re not knowledgeable enough in our understanding of what the bacteria are.”
Problematic probiotics
When considering giving probiotics to infants who seem healthy immediately after birth, Gibson urges caution. “If you don’t know what you’re intervening for, then I just wouldn’t do an intervention,” she says. And right now, she thinks that the data to support their use just aren’t there. “We don’t have enough information about what bacteria strains should be given at various developmental stages,” she says.
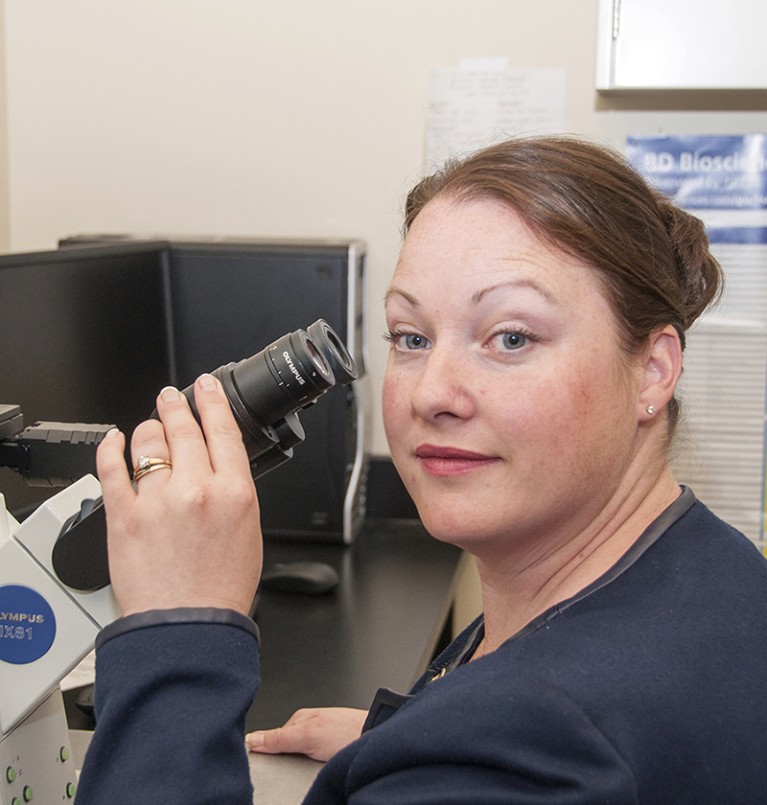
Deanna Gibson says that there is not enough data to support giving probiotics to infants.Credit: UBCO Photo
Most microbiome data come from people in North America and Europe, Gibson says, where disease incidence is on the rise. “Who’s to say that’s the most healthy population to study?,” she says. And even where there is evidence that probiotics might be beneficial, consumers have no assurance that the supplements they purchase deliver the microbes advertised. A 2021 study found that of 104 probiotic products, nearly half contained different bacteria from those listed on the label1. “That’s scary when you’re thinking about putting it in an infant,” says Gibson.
Parents giving probiotic supplements to their children, Gibson adds, have “been given the impression that those are the right microbes and that it’s okay to give your baby, you know, 12 billion counts of bacteria of one kind.” In 2018, she and her colleagues did an observational study that tracked the health of infants who were exposed to probiotics in the first six months of life either directly in supplements, indirectly in the milk of mothers taking a supplement, or both2. The researchers found only minimal changes to the gut microbiomes of these infants, but those who received probiotics had a higher rate of mucosal-associated illnesses as toddlers than did those not exposed to probiotics. “We’re moving way too fast in that area, without a lot of evidence and [with] too many assumptions,” Gibson says.
Under a watchful eye
No probiotic supplements can be sold as a drug for treating or preventing disease in the United States — instead, they are marketed as foods. Indeed, the only microbiome products to have run the rigorous FDA approvals gauntlet are those used in faecal microbiota transplantation (FMT): the transfer of faecal bacteria from a healthy donor into a recipient’s gastrointestinal tract.

Samples from stool bank OpenBiome are used for faecal microbiota transplantation.Credit: Jeff McIntosh/Associated Press/Alamy
FMT is highly effective in treating Clostridioides difficile infection, with a cure rate of 80–90% in both adults and children3. C. difficile is a bacterium that can cause diarrhoea and colon inflammation, and it is notoriously resistant to antibiotic treatment.
The FDA has approved the use of two FMT products — Rebyota in 2022 and Vowst in 2023 — for preventing the recurrence of C. difficile infection in adults. Rebyota is a filtered faecal preparation that is composed of microbes from a donor suspended in a solution and delivered rectally, whereas Vowst is an oral capsule. However, these products are not approved for children or for adults with other forms of the infection, such as fulminant C. difficile, which causes extreme inflammation of the colon and has a death rate of 34–80%. Because of this, “many patients are still undergoing traditional FMT, which is not FDA approved”, says gastroenterologist Lea Ann Chen at Rutgers University in New Brunswick, New Jersey.
The type of FMT Chen is referring to is, like Rebyota, a filtered faecal preparation from a donor. Most clinical practices use preparations from external stool banks such as OpenBiome in Woburn, Massachusetts. For years, the FDA has allowed such stool banks to bypass clinical trials to facilitate access for people who do not respond to standard therapies. But on 31 December, the FDA will end its enforcement discretion for OpenBiome, to the dismay and confusion of many patients and physicians.
Some adults with C. difficile infections are likely to see the cost of treatment increase. OpenBiome’s faecal microbiota preparation is much less expensive than the FDA-approved products, at roughly $1,700 per dose, compared with more than $9,000 for Rebyota and nearly $20,000 for Vowst (although many health-insurance plans will at least partially cover the cost of the two approved treatments).
For children, Reybota and Vowst are largely unavailable. “The pipeline for paediatric drug approval is very slow and usually lags 8–10 years behind adult approval,” says Kahn, who is director of the Fecal Microbiota Transplantation and Therapeutics Program at Boston Children’s Hospital. Physicians can make individual applications to the FDA to allow compassionate use of drugs in cases of life and death, but insurance companies might not cover the cost.
Internal stool banks — in hospitals, for example — will not be affected by the regulatory change, but Kahn still thinks that it will leave children with fewer options and “will also likely create a situation in which patients start doing home FMT, which is clearly not safe”.
Kahn, who has treated children as young as one, has seen first-hand the harm that can be done by FMT carried out at home with a kit purchased online. In one case, she recalls a child with inflammatory bowel disease (IBD) ending up in hospital after their abdominal pain and diarrhoea became worse after a home FMT from an unscreened family member. “You may feel like you’re making people better, but you’re really taking a huge risk, and you’re really compromising patient safety,” she says.
“The perception from patients, and probably also a good part of the medical community early on, was that faecal transplants are natural and therefore safe,” says Chen. And although publicized deaths due to FMT have made the immediate and acute risk more evident, long-term risk, such as the chance of developing diseases such as diabetes or cancer, is not yet understood. “This really tends to guide my clinical recommendations,” says Chen. For example, if a person in their 80s has a C. difficile infection, the short-term risk from infection outweighs any long-term risks and Chen will instigate a faecal transplant more quickly than she would for a younger person. For younger people, Chen says, she would instead typically offer another course of antibiotics first.
The success of FMT in treating C. difficile has led to it being considered as a therapeutic for a number of other illnesses, including ulcerative colitis, a form of IBD. When treating infants and young children — either as part of a clinical trial or under ‘compassionate use’, when a person has a serious or life-threatening illness — Kahn carefully considers the alternatives. With ulcerative colitis in particular, she says, a person who has not responded to three conventional therapies is unlikely to respond to a fourth. “At that point, their option is surgery.” So, despite the known acute risks and uncertain long-term consequences of FMT, “many patients and providers are asking, isn’t it better to have something to try if the alternative is so drastic?”
Walking a fine line
Kahn stresses the importance of physicians evaluating whether FMT or another microbiome intervention is right for their patient. But direct-to-consumer microbiome testing, in which people send faecal, oral or vaginal swab samples to companies for analysis, can bypass that ethical benchmark.
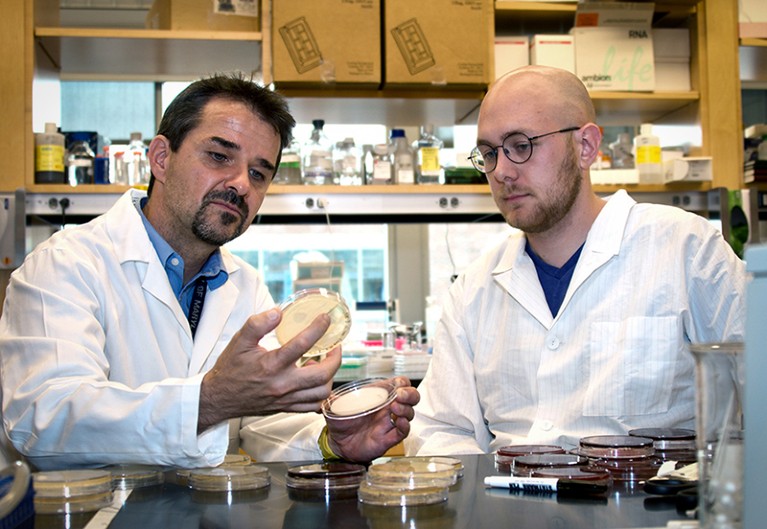
Jacques Ravel (left) says that consumers should be cautious about companies offering microbiome testing.Credit: Ravel Lab.
For nearly a decade, such test kits have allowed people to learn about the bacteria that make up their gut. For consumers who are simply curious, that’s no problem, says Jacques Ravel, a microbiome researcher at the University of Maryland, School of Medicine in Baltimore. More troubling is when test makers sell the promise of a diagnosis and suggested treatments, including expensive probiotic supplements made by the company itself.
Ravel and his colleagues think that these tests prey on the desperation of individuals, such as those with cases of IBD or bacterial vaginosis that physicians have not been able to treat. The tests are not subject to adverse event reporting in the way that approved clinical products are, making it difficult to assess the consequences of the advice that is doled out. But Ravel is aware of some anecdotal reports. For example, while in a focus group with physicians, he learnt of a patient who developed avoidant/restrictive food intake disorder after a microbiome test advised them to avoid certain foods.
Now, a growing number of direct-to-consumer microbiome tests are being marketed to parents for use with their infants. One company advertises “evidence-based insights and recommendations” in large font on its website, while simultaneously noting in smaller type at the foot of the page that its tests are “not intended to diagnose or treat disease”. “They are walking a fine line with respect to regulations and the law, and I suspect they know how to avoid fully stepping over it,” Ravel says.
Ravel thinks that there are a number of ways in which infant microbiome tests could inadvertently lead to harm. For instance, he says, if a test claims that a baby has low microbial diversity in their gut, a parent might try to introduce certain solid foods to rectify this too early, increasing the risk of digestive-system harm and allergies. A test that suggests specific supplements to enhance an infant’s health, meanwhile, might lead a parent to neglect important, evidence-based nutritional practices “in favour of unproven interventions”, Ravel adds. “Excessive reliance on supplements could interfere with natural growth and development.”
To reduce risk, Ravel thinks that there should be FDA-approved standards for microbiome analysis. “We had to do that for COVID-19. We have to do that for every single test that we use in medicine,” he says. For now, his advice is clear: “Parents should always consult their paediatrician before administering any product to their babies.”
Safety layers
Not all microbiome-based interventions directed at children are quite so ethically fraught. Vaginal seeding — in which vaginal fluids are transferred from a mother to the skin, mouth or nose of her newborn after a caesarean delivery — seems to effectively fortify the baby’s immune system and lower the risk of various immune and other diseases later in life.
The first interventional study of vaginal seeding was published in 2016 (ref. 4). Researchers showed that by swabbing babies born by caesarean with microbes from their mothers’ vaginas, they could give the baby a microbiome more similar to that of a baby born by vaginal delivery. “After that, there was this huge amount of interest from the press and mothers who were having c-sections, but there was a lot of appropriate caution as well,” says paediatric gastroenterologist Suchitra Hourigan, chief of the Clinical Microbiome Unit at the National Institutes of Health in Bethesda, Maryland. Hourigan recalls scepticism from the American College of Obstetricians and Gynecologists, and the broader community calling for large, controlled trials to show that vaginal seeding was in fact beneficial and safe. Today, Hourigan is a lead investigator on the largest vaginal seeding clinical trial so far, with an anticipated 600 babies born by c-section taking part. The trial is expected to finish in 2029.
Vaginal seeding is not FDA-approved, and there is debate over whether it should fall under FDA regulation at all, says Hourigan — if a baby is delivered vaginally, they would naturally be exposed to their mother’s vaginal fluid. “It’s actually the medical intervention of a c-section that interrupts this,” she says. Unlike a faecal transplant, in which the intention is to provide an individual with a microbiome that they would never otherwise have developed, Hourigan sees vaginal seeding as “an attempt to restore or replicate some of the exposures in a vaginal delivery”.
Trials require researchers to submit an application for an investigational new drug and to define what the drug they’re using is composed of. But this usually routine task is a challenge when the ‘drug’ is vaginal fluid. “It’s very hard to say because there’s so much variability,” says Hourigan. In the case of the large vaginal seeding trial, Hourigan and her colleagues submitted an application with three possible components of vaginal fluid, indicating that the exact composition would vary from mother to mother.
An FDA-regulated trial is the safest way to approach vaginal seeding, says Kahn, because it requires infectious-disease testing throughout pregnancy. “However, the request is made quite often by families undergoing c-section, and I think sometimes their request is granted or they do it themselves.” In one case of vaginal seeding done outside an approved trial, herpes simplex virus might have been passed from mother to baby5. “It is possible, in one of the trials, that would have been screened out before it could have happened,” says Hourigan. So far, there has been no reported transmission of infection in approved vaginal seeding trials.
As researchers work on developing safe and effective microbiome interventions to improve health, there is a lot of anticipation about what the future could hold. But that future should not be rushed, says Kahn. “Rarely in medicine do we have a magic pill for things,” she says. “We really need to understand the conditions for which treatments work, the conditions for which they don’t work, and how to keep advancing our knowledge and understanding.”
Greek Live Channels Όλα τα Ελληνικά κανάλια:
Βρίσκεστε μακριά από το σπίτι ή δεν έχετε πρόσβαση σε τηλεόραση;
Το IPTV σας επιτρέπει να παρακολουθείτε όλα τα Ελληνικά κανάλια και άλλο περιεχόμενο από οποιαδήποτε συσκευή συνδεδεμένη στο διαδίκτυο.
Αν θες πρόσβαση σε όλα τα Ελληνικά κανάλια
Πατήστε Εδώ
Ακολουθήστε το TechFreak.GR στο Google News για να μάθετε πρώτοι όλες τις ειδήσεις τεχνολογίας.





